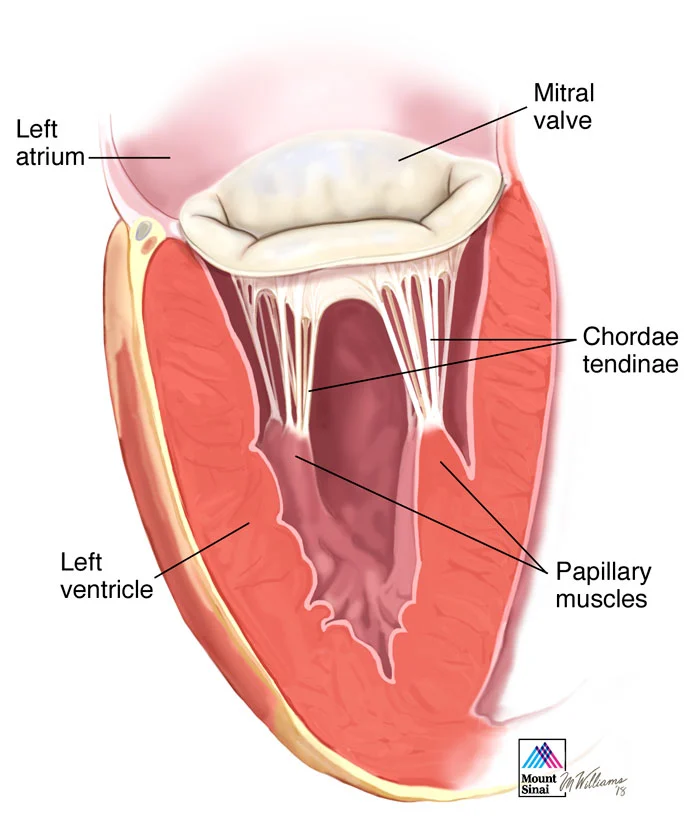
The mitral valve is one of four valves in the heart that keep blood flowing in the right direction. Each valve has flaps (leaflets) that open and close once during each heartbeat. If a valve doesn't open or close properly, blood flow through the heart to the body can be reduced.
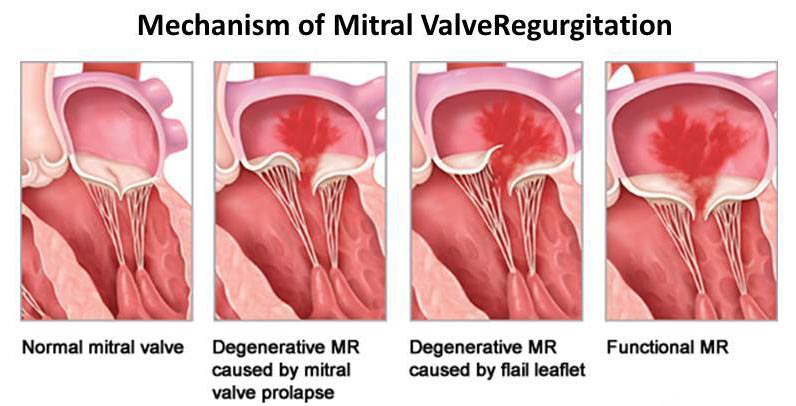
In mitral valve regurgitation, the flaps don't close tightly. Blood flows backward when the valve is closed, making it harder for the heart to work properly.
In mitral valve stenosis, the valve opening narrows. The heart now must work harder to force blood through the smaller valve opening. If the opening in the valve becomes small enough, it can reduce blood flow from the left atrium to the left ventricle.
Mitral valve disease has many causes. Some forms of mitral valve disease can be present at birth (congenital heart defect).
Mitral valve disease may also develop later in life (acquired). For example, mitral valve stenosis is often caused by rheumatic fever. This fever is a complication of a strep infection that can affect the heart. When this happens, it's called rheumatic mitral valve disease.
Other causes of acquired mitral valve disease include:
- Other heart conditions
- Infection
- Age-related changes
- Autoimmune disease, such as lupus
Mitral valve repair
Mitral valve repair is based on the identification of the mechanism of the mitral regurgitation: Annular dilatation, chordal rupture, chordal elongation, leaflet perforation, leaflet prolapse, flail leaflet, dialated cardiomyopathy.
Mitral valve repair is better for long term function of the heart and also avoids the need for anticoaguliton medicines.
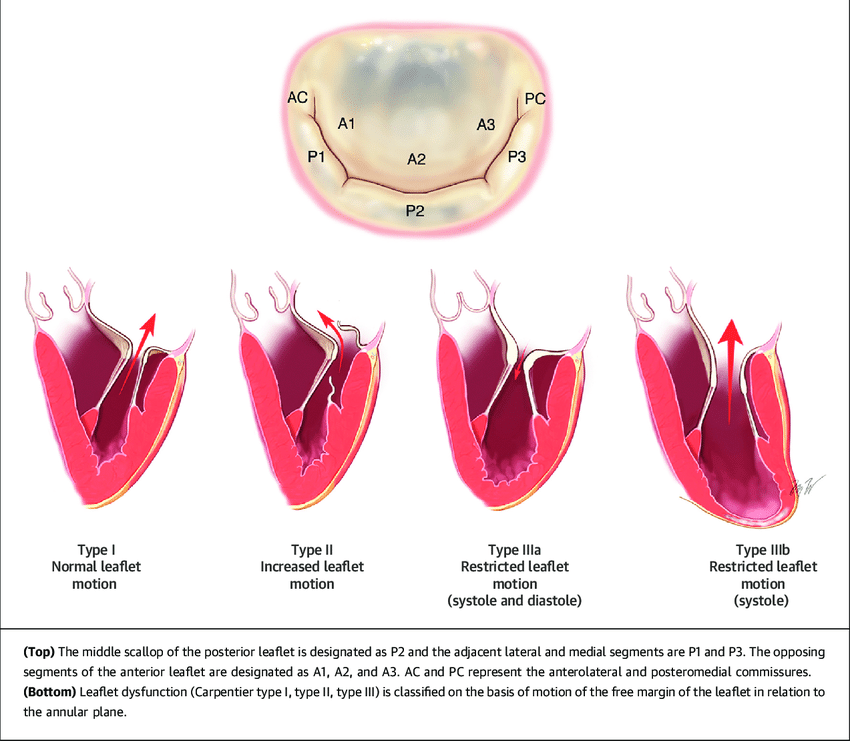
Diagnosis and indications for mitral valve repair surgery are based on echocardiography analysis to quantify the regurgitation and to identify the mechanism.
Various techniques are used to achieve a successful mitral valve repair. Posterior leaflet prolapse due to fibroelastic deficiency is most common cause of severe mitral regurgitation and it is classically treated by a resection of the prolapsed segment affected by chordal rupture or elongation.
The prolapsed segment is removed by excising a quadrangular or triangular portion of the leaflet. The posterior annulus is then vertically plicated by placing and tying several sutures in the resected area. Direct suturing of the leaflet remnants restores posterior leaflet continuity. In some situations the resection is extended along the annulus in order to downsize the height of the posterior leaflet as a sliding plasty.
The alternative to the resection of the tissue is the implantation of artificial chordae between the papillary muscle and the free edge of the leaflet in order to restore a good position of the leaflet; this technique respects the tissue and the mobility of the leaflet.
Finally, a remodeling ring annuloplasty restores the physiologic ratio of the normal annulus; not only the size but also the shape of the annulus. An annuloplasty ring prevents further annular dilatation, preserves leaflet mobility, and relieves tension on the leaflets (stabilizing the repair) by optimizing the coaptation zone.
An annuloplasty is performed by first placing horizontal mattress sutures circumferentially through the annulus. Appropriate ring sizing is then based on measuring the inter-commissural distance and also the surface area of the anterior leaflet, using sizers correlated to normal mitral geometry.

Mitral Valve replacement
When Valve repair is not appropriate (endocarditis, calcifications), or not possible (most often in rheumatic disease), the option of valve replacement with bioprosthesis or mechanical valve remains the alternative. The leaflets are removed and then the prosthesis is implanted with stiches fixed on the mitral annulus.
